On Ketamine
The Hippies Were On To Something
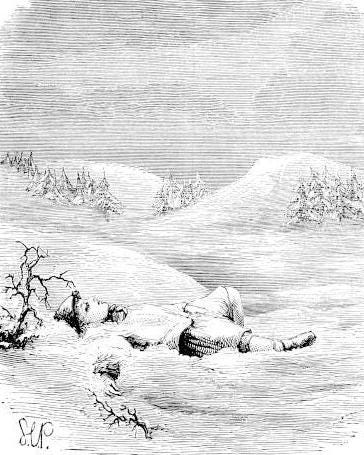
If the world were to shatter and fall on him, its ruins would strike him, but fear would not. - Horace
Ketamine is a drug that's been available in the United States for a long time, more than 50 years. Since its synthesis in a Detroit laboratory nearly six decades ago, ketamine has proven to be a complex medication with unusual properties, heterogeneous,…